The Silent Storytellers: Why Your Observation Notes Are a Lifesaver (Literally)
Let’s be honest. When you’re rushing between shifts, helping a client shower, preparing a meal, and trying to keep the conversation flowing, stopping to record a blood pressure reading or a bowel chart can feel like just another box to tick.
It’s easy to think, “I’ll just write down the numbers, and the office will deal with it.”
But here is the truth: You are the eyes and ears of the healthcare system.
Doctors see a patient for 15 minutes once a month. You see them every day. The notes you take aren't just "admin"—they are the early warning system that keeps your client safe, comfortable, and out of the hospital.
Here is a breakdown of why specific observations matter, and the real-life moments when they become critical.
1. Blood Pressure & Pulse: The "Silent" Alarm
High blood pressure (hypertension) rarely hurts. A client can be walking around with dangerously high BP and feel totally fine—until they aren't.
● When is this crucial?
○ The "Woozy" Moment: If a client says they feel a bit dizzy when they stand up, checking their BP immediately tells us if they are a fall risk (Postural Hypotension).
○ Medication Changes: If the GP has just started them on new heart meds, your daily log proves if the pills are working or if the dose is too strong.
○ The "Off" Day: Sometimes a client just seems quiet or flushed. A quick pulse and BP check can reveal an infection or heart irregularity before it becomes an emergency
.
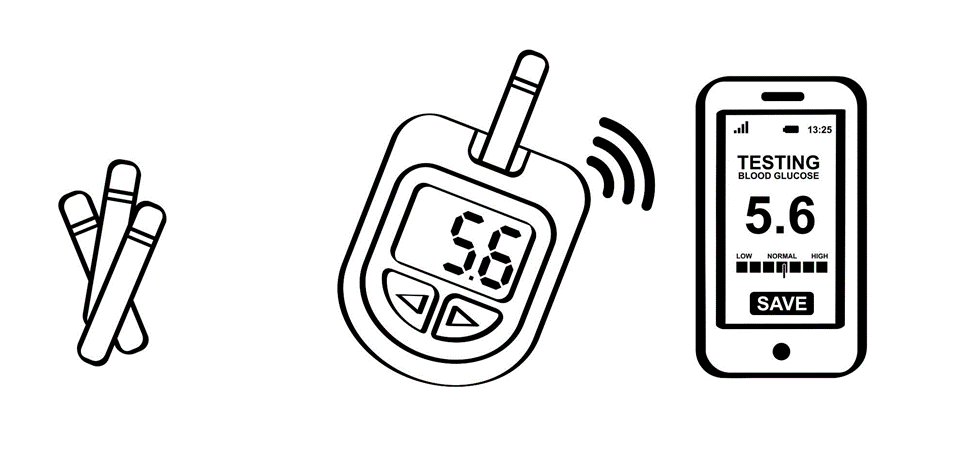
2. Blood Sugar Levels (BGL): The Mood & Safety Check
For clients with diabetes, blood sugar is the fuel in their tank. Too much or too little, and the engine starts to sputter.
● When is this crucial?
○ The "Behavior" Shift: Have you ever had a client who is usually sweet become suddenly aggressive, confused, or lethargic? Before assuming it’s dementia or a bad mood, check their BGL. Low sugar (Hypo) often looks like confusion. A jelly bean might be the cure.
○ Wound Healing: If you notice a cut on their leg isn't healing, consistent high blood sugar might be the culprit. Your records help the nurse spot this link.
Shutterstock
3. Weight: The Long-Term Detective
Stepping on the scales seems mundane, but weight is one of the best indicators of overall health in Aged Care and disability.
● When is this crucial?
○ The "Fluid" Red Flag: If a client gains 2kg in a single week, it’s not fat—it’s fluid. This is a classic sign of heart failure. Your record prompts the doctor to adjust their diuretics immediately, potentially stopping a hospital admission for fluid on the lungs.
○ The Silent Decline: Gradual weight loss over months can be a sign of ill-fitting dentures, depression, or difficulty swallowing. Spotting the trend early means we can get a Dietitian involved before they become frail.
4. Turning & Skin Charts: The Dignity Protectors
For participants who are bed-bound or use a wheelchair, their skin is their first line of defense.
● When is this crucial?
○ The "Hidden" Pain: A pressure injury (bed sore) can form in just a few hours. Once the skin breaks, it is incredibly painful and prone to infection.
○ Proof of Care: A turning chart isn't just about skin; it’s about comfort. It proves that we are respecting the person’s dignity by ensuring they aren't lying in the same position, stiff and sore, for hours on end.
The Takeaway
Next time you pull out your phone or tablet to log a vital sign, remember: You aren't just entering data.
You are telling the story of that person's health. You are the one spotting the infection, preventing the fall, and ensuring their comfort.
Tools make it easier to record, but it’s your attention to detail that makes the difference.
________________________________________
Keep up the great work, legends!